Why Do I Have Hallux Valgus?
Overview
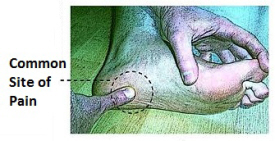
 Bunions, Corns, and Calluses are common foot ailments associated with improperly-fitted footwear. Please contact your family doctor or Podiatrist to ask them how Birkenstock footwear or arch supports can help treat your symptoms. Also, feel free to contact your local Birkenstock retailer about their healthy footwear recommendations. Birkenstock has many products that can help with Bunions, Corns, and Calluses. Bunions are a prominent bump on the inside of the foot around the big toe joint. Corns are an accumulation of dead skin cells usually found on the toes, forming thick hardened areas. They contain a cone-shaped core whose point can press on a nerve below causing pain. Calluses are also an accumulation of dead skin cells that harden and thicken over an area of the foot. They are the body?s defense mechanism against excessive pressure and friction. Calluses are normally found on the bottom of the foot, the heel, and/or the inside of the big toe.
Bunions, Corns, and Calluses are common foot ailments associated with improperly-fitted footwear. Please contact your family doctor or Podiatrist to ask them how Birkenstock footwear or arch supports can help treat your symptoms. Also, feel free to contact your local Birkenstock retailer about their healthy footwear recommendations. Birkenstock has many products that can help with Bunions, Corns, and Calluses. Bunions are a prominent bump on the inside of the foot around the big toe joint. Corns are an accumulation of dead skin cells usually found on the toes, forming thick hardened areas. They contain a cone-shaped core whose point can press on a nerve below causing pain. Calluses are also an accumulation of dead skin cells that harden and thicken over an area of the foot. They are the body?s defense mechanism against excessive pressure and friction. Calluses are normally found on the bottom of the foot, the heel, and/or the inside of the big toe.
Causes
Shoes. The primary cause of bunions is the long term use of shoes, particularly tight-fitting shoes with pointed toes, or high heeled shoes. A study that examined people in cultures that do not wear shoes found no cases of bunions. Genetic. People who have misaligned toes or feet, are flatfooted with feet that roll inwards (over pronation), excessive flexibility of ligaments, abnormal bone structure, or have mechanical instability in the big toe joint are more susceptible to bunions. This is especially common when bunions occur in children or young adults. Injuries or other trauma (sprains, fractures or nerve injuries), neuromuscular disorders (polio or Charcot-Marie-Tooth disease), or limb-length discrepancies (one leg longer than the other). Repetitive stresses to the foot. Bunions are common in ballet dancers and in a few sports. Arthritis.
Symptoms
Movement of the big toe towards the smaller toes. Bulging bump on the outside of the base of the big toe. Restricted movement of the big toe. Swelling, inflammation, redness or soreness around your big toe joint. Persistent or sporadic dull, sharp or aching pain in or around the big toe. Corns, blisters and calluses which can develop when the first and second toes overlap. Over time, more severe symptoms can occur such as arthritis of the big toe, stress fractures and problems walking.
Diagnosis
Your family doctor or chiropodist /podiatrist can identify a bunion simply by examining your foot. During the exam, your big toe will be moved up and down to determine if your range of motion is limited. You will be examined for signs of redness or swelling and be questioned about your history of pain. A foot x-ray can show an abnormal angle between the big toe and the foot. In some cases, arthritis may also be seen. A X-ray of your foot may help identify the cause of the bunion and rate its severity.
Non Surgical Treatment
Most of the time, non-surgical (conservative) treatment can control the symptoms of a foot bunion or bunionette. These include. Appropriate Footwear, changing to wide fitting footwear reduces the pressure on the big toe and prevents shoes from rubbing on the bony lump. When possible, go barefoot Toe stretchers are a really simple way to reduce foot bunion pain. Toe Stretchers, wearing toe spaces that fit in-between the toes help to stretch the muscles and ligaments around the toes, improving the alignment and relieving pain. Find out more about how these work in the Toe Stretcher section. Painkillers, your doctor may prescribe or recommend over-the-counter medication to reduce the pain and inflammation. Foot bunion correctors can be worn in your shoe to help realign your foot if you suffer from foot bunions. Orthotics. There are a number of over-the-counter shoe inserts that can help relieve symptoms. Bunion correctors work by realigning the bones in your foot to reduce pressure on the affected toe. There are both day-time and night-time splints on the market, although the evidence of their effectiveness is lacking. Ice. Applying ice packs to the foot can help reduce pain and inflammation. Bunion pads help to reduce any friction on your big toe. Bunion Pads. You can also get protective foot cushions that sit over the skin to prevent the hallux abducto valgus rubbing on your shoes. 
Surgical Treatment
Bunion surgery is usually done as an out patient procedure, so the patient does not have to stay in hospital overnight although it is usually performed under a general anesthetic. The procedure involves the surgeon making a cut on the inside of the big toe joint and removing excess bone whilst also repositioning ligaments and tendons. The joint may be fixed with screws or wires, which may be dissolve, or may be removed at a later date or in some cases, remain in the foot permanently. After the operation the foot will be immobilized, often in a cast for 4 to 8 weeks to keep the bones in alignment. Crutches will usually be issued to help the patient get around. After this period, the foot will be assessed to check the bones have healed correctly. At which point full weight bearing may be gradually introduced.
Prevention
Shoes that possess tapering toe boxes should be avoided if you have a bunion, as narrow toe boxes will hasten the progression of your bunion deformity. In some cases, conservative measures, including switching to appropriate footwear, may not have the desired effect, and your podiatrist may recommend for you a surgical procedure known as a bunionectomy.
The Truth About Over-Pronation
Over pronation of the foot is commonly referred to as "flat feet." Many middle-aged men and women suffer from over pronation over time and as a result of wearing poor-fitting shoes, continuing with repetitive exercising habits, or walking in high heels for long periods over several years. Regular speed-walkers often experience over pronation as well as a result of this activity.

Causes
It is important to identify the cause of overpronation in order to determine the best treatment methods to adopt. Not all treatments and preventative measures will work equally well for everyone, and there may be a little trial and error involved to get the best treatment. A trip to a podiatrist or a sports therapist will help you to establish the cause of overpronation, and they will be able to tell you the best treatments based on your specific degree of overpronation and the cause. Overpronation has many causes, with the most common reasons for excessive pronation listed, low arches, flexible flat feet, fallen arches, gait abnormalities, abnormal bone structure, abnormal musculature, bunions, corns and calluses.
Symptoms
If you overpronate, your symptoms may include discomfort in the arch and sole of foot. Your foot may appear to turn outward at the ankle. Your shoes wear down faster on the medial (inner) side of your shoes. Pain in ankle, shins, knees, or hips, especially when walking or running.Unfortunately, overpronation can lead to additional problems with your feet, ankles, and knees. Runners in particular find that overpronation can lead to shin splints, tarsal tunnel syndrome, plantar fasciitis, compartment syndrome, achilles tendonitis, bunions (hallux valgus) patello femoral pain syndrome, heel spurs, metatarsalgia. You do not have to be a runner or athlete to suffer from overpronation. Flat feet can be inherited, and many people suffer from pain on a day-to-day basis. Flat feet can also be traumatic in nature and result from tendon damage over time. Wearing shoes that do not offer enough arch support can also contribute to overpronation.
Diagnosis
You can test for pronation by looking at the leg and foot from the back. Normally you can see the Achilles Tendon run straight down the leg into the heel. If the foot is pronated, the tendon will run straight down the leg, but when it lies on the heel it will twist outward. This makes the inner ankle bone much more prominent than the outer ankle bone.

Non Surgical Treatment
When you see the doctor, he or she will likely perform a complete examination of your feet and watch you walk. The doctor will need to take x-rays to determine the cause of your flat feet. In some cases, further imaging may be needed, especially if your symptoms are severe and sudden in nature. Once you are properly diagnosed, your doctor will create an appropriate treatment plan. There are several options to correct overpronation, such as orthotics. In many cases, overpronation can be treated with non-surgical methods and over-the-counter orthotics. In severe cases, however, custom-made orthotics may work better. Orthotics provide arch support and therefore prevent collapse of the arch with weight bearing. They are made of materials such as spongy rubber or hard plastic. Your doctor will also want to examine your footwear to ensure they fit properly and offer enough medial support. Extra support and stability can be achieved with footwear that has a firm heel counter. If you are experiencing pain, you should be able to use over-the-counter pain medications such as ibuprofen to relieve symptoms.
Surgical Treatment
HyProCure implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
Physiotherapy For Severs Disease
Sever disease refers to a calcaneal apophysitis (an inflammation of the apophysis of the heel) which occurs in children and young adolescents. It typically presents in active young children (especially ones who engage in jumping and running sports).
Causes
At birth, most of our foot bones are still made of cartilage, which ossifies (becomes bony) over the first few years of life. At the back of the heel, there is a growth plate that is attached to the main body of the heel bone by a cartilaginous join. At about the age of 14-15 years, this area of cartilage between the growth plate and the heel bone ossifies, fusing the area to the heel. Sever?s disease occurs when there is too much motion or strain across the growth plate, resulting in this area becoming inflamed and painful.
Symptoms
The most common symptoms of Sever?s involves pain or tenderness in one or both heels. This pain usually occurs at the back of the heel, but can also extend to the sides and bottom of the heel. A child with Sever?s may also have these common problems, Heel pain with limping, especially after running. Difficulty walking, Discomfort or stiffness in the feet upon awaking. Swelling and redness in the heel, Symptoms are usually worse during or after activity and get better with rest.
Diagnosis
It is not difficult for a doctor to diagnose Sever's disease in a youngster or teenager. A personal history and a physical examination are usually all it takes to determine the cause of heel pain.
Non Surgical Treatment
stretching exercises can help. It is important that your child performs exercises to stretch the hamstring and calf muscles, and the tendons on the back of the leg. The child should do these stretches 2 or 3 times a day. Each stretch should be held for about 20 seconds. Both legs should be stretched, even if the pain is only in 1 heel. Your child also needs to do exercises to strengthen the muscles on the front of the shin. To do this, your child should sit on the floor, keeping his or her hurt leg straight. One end of a bungee cord or piece of rubber tubing is hooked around a table leg. The other end is hitched around the child's toes. The child then scoots back just far enough to stretch the cord. Next, the child slowly bends the foot toward his or her body. When the child cannot bend the foot any closer, he or she slowly points the foot in the opposite direction (toward the table). This exercise (15 repetitions of "foot curling") should be done about 3 times. The child should do this exercise routine a few times daily.
Acquired Flat Foot Tibialis Posterior Dysfunction
Overview
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot. PTTD is often called ?adult acquired flatfoot? because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it isn?t treated early. 
Causes
There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. The most common cause of acquired adult flatfoot is posterior tibial tendon dysfunction.
Symptoms
Posterior tibial tendon insufficiency is divided into stages by most foot and ankle specialists. In stage I, there is pain along the posterior tibial tendon without deformity or collapse of the arch. The patient has the somewhat flat or normal-appearing foot they have always had. In stage II, deformity from the condition has started to occur, resulting in some collapse of the arch, which may or may not be noticeable. The patient may feel it as a weakness in the arch. Many patients initially present in stage II, as the ligament failure can occur at the same time as the tendon failure and therefore deformity can already be occurring as the tendon is becoming symptomatic. In stage III, the deformity has progressed to the extent where the foot becomes fixed (rigid) in its deformed position. Finally, in stage IV, deformity occurs at the ankle in addition to the deformity in the foot.
Diagnosis
First, both feet should be examined with the patient standing and the entire lower extremity visible. The foot should be inspected from above as well as from behind the patient, as valgus angulation of the hindfoot is best appreciated when the foot is viewed from behind. Johnson described the so-called more-toes sign: with more advanced deformity and abduction of the forefoot, more of the lateral toes become visible when the foot is viewed from behind. The single-limb heel-rise test is an excellent determinant of the function of the posterior tibial tendon. The patient is asked to attempt to rise onto the ball of one foot while the other foot is suspended off the floor. Under normal circumstances, the posterior tibial muscle, which inverts and stabilizes the hindfoot, is activated as the patient begins to rise onto the forefoot. The gastrocnemius-soleus muscle group then elevates the calcaneus, and the heel-rise is accomplished. With dysfunction of the posterior tibial tendon, however, inversion of the heel is weak, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If the patient can do a single-limb heel-rise, the limb may be stressed further by asking the patient to perform this maneuver repetitively.
Non surgical Treatment
Patients can be treated non-surgically with in-shoe devices and braces to hold their feet in the correct position. This can reduce pain and damage and assist with walking. Physical therapy is also given to improve muscle strength and help prevent injury to the foot. Surgery can be performed if the patient doesn?t find any relief. 
Surgical Treatment
If cast immobilization fails, surgery is the next alternative. Treatment goals include eliminating pain, halting deformity progression and improving mobility. Subtalar Arthroereisis, 15 minute outpatient procedure, may correct flexible flatfoot deformity (hyperpronation). The procedure involves placing an implant under the ankle joint (sinus tarsi) to prevent abnormal motion. Very little recovery time is required and it is completely reversible if necessary. Ask your Dallas foot doctor for more information about this exciting treatment possibility.
What Causes Heel Soreness

More than 20 percent of patients visit foot specialists because of Heel Pain, and approximately one-third of all patients I see come because of this problem. Over 50 percent of Americans will experience heel pain during their lifetime. The most common form of heel pain is known as plantar fasciitis or "heel spur syndrome." The plantar fascia is a thick ligament on the bottom of your foot spanning from your heel to the base of your toes. It supports the arch and several muscles under the bones that support the foot. Overtime, most people will develop some degree of calcification within these muscles on the bottom of their heel called a "spur."
Causes
In our pursuit of healthy bodies, pain can be an enemy. In some instances, however, it is of biological benefit. Pain that occurs right after an injury or early in an illness may play a protective role, often warning us about the damage we've suffered. When we sprain an ankle, for example, the pain warns us that the ligament and soft tissues may be frayed and bruised, and that further activity may cause additional injury. Pain, such as may occur in our heels, also alerts us to seek medical attention. This alert is of utmost importance because of the many afflictions that contribute to heel pain.
Symptoms
Pain typically comes on gradually, with no injury to the affected area. It is frequently triggered by wearing a flat shoe, such as flip-flop sandals. Flat footwear may stretch the plantar fascia to such an extent that the area becomes swollen (inflamed). In most cases, the pain is under the foot, toward the front of the heel. Post-static dyskinesia (pain after rest) symptoms tend to be worse just after getting out of bed in the morning, and after a period of rest during the day. After a bit of activity symptoms often improve a bit. However, they may worsen again toward the end of the day.
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests.
Non Surgical Treatment
Treatment for plantar fasciitis - the vast majority of patients recover with conservative treatments (designed to avoid radical medical therapeutic measures or operative procedures) within months. Heel with ice-pack. Home care such as rest, ice-pack use, proper-fitting footwear and foot supports are often enough to ease heel pain. Non-steroidal anti-inflammatory drugs (NSAIDs) - medications with analgesic (pain reducing), antipyretic (fever reducing) effects. In higher doses they also have anti-inflammatory effects, they reduce inflammation (swelling). Non-steroidal distinguishes NSAIDs from other drugs which contain steroids, which are also anti-inflammatory. NSAIDs are non-narcotic (they do not induce stupor). For patients with plantar fasciitis they may help with pain and inflammation. Corticosteroids, a corticosteroid solution is applied over the affected area on the skin; an electric current is used to help absorption. Alternatively, the doctor may decide to inject the medication. However, multiple injections may result in a weakened plantar fascia, significantly increasing the risk of rupture and shrinkage of the fat pad covering the heel bone. Some doctors may use ultrasound to help them make sure they have injected in the right place Corticosteroids are usually recommended when NSAIDs have not helped. Physical therapy, a qualified/specialized physical therapist (UK: physiotherapist) can teach the patient exercises which stretch the plantar fascia and Achilles tendon, as well as strengthening the lower leg muscles, resulting in better stabilization of the ankle and heel. The patient may also be taught how to apply athletic taping, which gives the bottom of the foot better support. Night splints, the splint is fitted to the calf and foot; the patient keeps it on during sleep. Overnight the plantar fascia and Achilles tendon are held in a lengthened position; this stretches them. Orthotics, insoles and orthotics (assistive devices) can be useful to correct foot faults, as well as cushioning and cradling the arch during the healing process. Extracorporeal shock wave therapy, sound waves are aimed at the affected area to encourage and stimulate healing. This type of therapy is only recommended for chronic (long-term) cases, which have not responded to conservative therapy.
Surgical Treatment
When a diagnosis of plantar fasciitis is made early, most patients respond to conservative treatment and don?t require surgical intervention. Often, when there is a secondary diagnosis contributing to your pain, such as an entrapped nerve, and you are non-responsive to conservative care, surgery may be considered. Dr. Talarico will discuss all options and which approach would be the most beneficial for your condition.
Prevention
It may not be possible to prevent all cases of heel pain. However, there are some easy steps that you can take to avoid injury to the heel and prevent pain. Whenever possible, you should wear shoes that fit properly and support the foot, wear the right shoes for physical activity, stretch your muscles before exercising, pace yourself during physical activity, maintain a healthy diet, rest when you feel tired or when your muscles ache, maintain a healthy weight.
What's The Major Cause Of Achilles Tendonitis ?
 Achilles tendonitis is an iInflammation in the tendon of the calf muscle, where it attaches to the heel bone. Achilles tendonitis causes pain and stiffness at the back of the leg, near the heel. Achilles tendonitis can be caused by overuse of the Achilles tendon, overly tight calf muscles or Achilles tendons, excess uphill running, a sudden increase in the intensity of training or the type of shoes worn to run, or wearing high heels at work and then switching to a lower-heeled workout shoe. Achilles tendonitis causes pain, tenderness, and often swelling over the Achilles tendon. There is pain on rising up on the toes and pain with stretching of the tendon. The range of motion of the ankle may be limited. Treatment includes applying ice packs to the Achilles tendon, raising the lower leg, and taking an anti-inflammatory medication. In some severe cases of Achilles tendonitis, a cast may be needed for several weeks. A heel lift insert may also be used in shoes to prevent future overstretching of the Achilles tendon. Exerting rapid stress on the Achilles tendon when it is inflamed can result in rupture of the tendon.
Achilles tendonitis is an iInflammation in the tendon of the calf muscle, where it attaches to the heel bone. Achilles tendonitis causes pain and stiffness at the back of the leg, near the heel. Achilles tendonitis can be caused by overuse of the Achilles tendon, overly tight calf muscles or Achilles tendons, excess uphill running, a sudden increase in the intensity of training or the type of shoes worn to run, or wearing high heels at work and then switching to a lower-heeled workout shoe. Achilles tendonitis causes pain, tenderness, and often swelling over the Achilles tendon. There is pain on rising up on the toes and pain with stretching of the tendon. The range of motion of the ankle may be limited. Treatment includes applying ice packs to the Achilles tendon, raising the lower leg, and taking an anti-inflammatory medication. In some severe cases of Achilles tendonitis, a cast may be needed for several weeks. A heel lift insert may also be used in shoes to prevent future overstretching of the Achilles tendon. Exerting rapid stress on the Achilles tendon when it is inflamed can result in rupture of the tendon.
Causes
Hill running or stair climbing. Overuse resulting from the natural lack of flexibility in the calf muscles. Rapidly increasing mileage or speed. Starting up too quickly after a layoff. Trauma caused by sudden and hard contraction of the calf muscles when putting out extra effort such as in a final sprint. Achilles tendinitis often begins with mild pain after exercise or running that gradually worsens.
Symptoms
Common symptoms of Achilles tendinitis include, pain and stiffness along the Achilles tendon in the morning, pain along the tendon or back of the heel that worsens with activity, Severe pain the day after exercising, thickening of the tendon, bone spur (insertional tendinitis) swelling that is present all the time and gets worse throughout the day with activity, If you have experienced a sudden "pop" in the back of your calf or heel, you may have ruptured (torn) your Achilles tendon. See your doctor immediately if you think you may have torn your tendon.
Diagnosis
The diagnosis is made via discussion with your doctor and physical examination. Typically, imaging studies are not needed to make the diagnosis. However, in some cases, an ultrasound is useful in looking for evidence of degenerative changes in the tendon and to rule out tendon rupture. An MRI can be used for similar purposes, as well. Your physician will determine whether or not further studies are necessary.
Nonsurgical Treatment
To help heal your Achille?s Tendinitis, follow the R.I.C.E. Principle including Rest, Ice Compression and Elevation. In addition your physiotherapist will likely recommend specific exercises promote healing and strengthening of the Achilles tendon and its supporting structures. As well an orthotic that elevates your heel can reduce stress on your Achilles tendon. Reducing inflammation in the tendon is important too this can often be achieved with oral pills or topical creams. Over-the-counter pain medications or prescription strength such as ibuprofen. However, these drugs can have side effects, like an increased risk of bleeding ulcers. They should be used only occasionally unless your doctor specifically says otherwise. Topical anti-inflammatory creams made with natural ingredients designed specifically for feet and legs (eg ZAX?s Original Heelspur Cream ) target the affected areas and provides effective and safe relief. Tendinitis usually responds well to self-care measures. But if your signs and symptoms are severe or persistent, your doctor might suggest other treatment options including surgery.

Surgical Treatment
Histological and biological studies on tendon healing have made it possible to envisage surgical repair using a percutaneous approach, with the following objectives, a minimal, and not very aggressive, operation, which is quick and easy and within the capabilities of all surgeons, the shortest hospitalisation period possible, above all, early and effective re-education, providing a satisfactory result both in terms of solidity and the comfort of the patient. The percutaneous tenosynthesis TENOLIG combines stability, reliability, patient comfort and lower overall social and professional costs for this type of lesion.
Prevention
If you're just getting started with your training, be sure to stretch after running, and start slowly, increasing your mileage by no more than 10% per week. Strengthen your calf muscles with exercises such as toe raises. Work low-impact cross-training activities, such as cycling and swimming, into your training.
What Is Painful Heel

Overview
Plantar fasciitis is a very common condition resulting in pain under the heel which often radiates into the foot. We explain free of charge everything you need to know to cure your pain and prevent it from returning.
Causes
You are more likely to develop plantar fasciitis if you are Active, sports that place excessive stress on the heel bone and attached tissue, especially if you have tight calf muscles or a stiff ankle from a previous ankle sprain, which limits ankle movement eg. Running, ballet dancing and aerobics. Overweight. Carrying around extra weight increases the strain and stress on your plantar fascia. Pregnant. The weight gain and swelling associated with pregnancy can cause ligaments to become more relaxed, which can lead to mechanical problems and inflammation. On your feet. Having a job that requires a lot of walking or standing on hard surfaces ie factory workers, teachers and waitresses. Flat Feet or High Foot Arches. Changes in the arch of your foot changes the shock absorption ability and can stretch and strain the plantar fascia, which then has to absorb the additional force. Middle-Aged or Older. With ageing the arch of your foot may begin to sag - putting extra stress on the plantar fascia. Wearing shoes with poor support. Weak Foot Arch Muscles. Muscle fatigue allows your plantar fascia to overstress and cause injury. Arthritis. Some types of arthritis can cause inflammation in the tendons in the bottom of your foot, which may lead to plantar fasciitis. Diabetes. Although doctors don't know why, plantar fasciitis occurs more often in people with diabetes.
Symptoms
Plantar fasciitis sufferers feel a sharp stab or deep ache in the middle of the heel or along the arch. Another sign is the morning hobble from the foot trying to heal itself in a contracted position overnight. Taking that first step causes sudden strain on the bottom of the foot. The pain can recur after long spells of sitting, but it tends to fade during a run, once the area is warmed up.
Diagnosis
To diagnose plantar fasciitis, your doctor will physically examine your foot by testing your reflexes, balance, coordination, muscle strength, and muscle tone. Your doctor may also advise a magnetic resonance imaging (MRI) or X-ray to rule out other others sources of your pain, such as a pinched nerve, stress fracture, or bone spur.
Non Surgical Treatment
Reducing inflammation in the plantar fascia ligament is an important part of treatment, though this does not address the underlying damage to the ligament. Initial home treatment includes staying off your feet and applying ice for 15 to 20 minutes three or four times a day to reduce swelling. You can also try reducing or changing your exercise activities. Using arch supports in your shoes and doing stretching exercises may also help to relieve pain. Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen (i.e. Motrin or Advil) and naproxen (i.e. Aleve), are often used to reduce inflammation in the ligament. If home treatments and over-the-counter anti-inflammatory drugs don’t ease the pain, an injection of a corticosteroid directly into the damaged section of the ligament can be given. Your doctor can do this in his or her office. Your doctor may use an ultrasound device to help determine the best place for the injection. Corticosteroids can also be administered on the skin of your heel or the arch of your foot, and then a painless electrical current is applied to let the steroid pass through your skin and into the muscle. Physical therapy is an important part of treatment for planter fasciitis. It can help stretch your plantar fascia and Achilles tendons. A physical therapist can also show you exercises to strengthen your lower leg muscles, helping to stabilize your walk and lessen the workload on your plantar fascia. If pain continues and other methods aren’t working, your doctor may recommend extracorporeal shock wave therapy. Sound waves are bombarded against your heel to stimulate healing within the ligament. This treatment can result in bruises, swelling, pain, and numbness, and has not been proven to be consistently effective in relieving symptoms.
Surgical Treatment
Surgery should be reserved for patients who have made every effort to fully participate in conservative treatments, but continue to have pain from plantar fasciitis. Patients should fit the following criteria. Symptoms for at least 9 months of treatment. Participation in daily treatments (exercises, stretches, etc.). If you fit these criteria, then surgery may be an option in the treatment of your plantar fasciitis. Unfortunately, surgery for treatment of plantar fasciitis is not as predictable as a surgeon might like. For example, surgeons can reliably predict that patients with severe knee arthritis will do well after knee replacement surgery about 95% of the time. Those are very good results. Unfortunately, the same is not true of patients with plantar fasciitis.
Stretching Exercises
Calf stretch. Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch. Plantar fascia stretch. This stretch is performed in the seated position. Cross your affected foot over the knee of your other leg. Grasp the toes of your painful foot and slowly pull them toward you in a controlled fashion. If it is difficult to reach your foot, wrap a towel around your big toe to help pull your toes toward you. Place your other hand along the plantar fascia. The fascia should feel like a tight band along the bottom of your foot when stretched. Hold the stretch for 10 seconds. Repeat it 20 times for each foot. This exercise is best done in the morning before standing or walking.